Discovery
How do people obtain their medication and can technology improve this journey? Should a product / service be built in-house or should our findings and recommendations be passed to third parties to develop their own solution? I led this discovery to uncover the answers to these questions.
TL;DR
NHS Digital | Medicines and Pharmacy
Patients in England that regularly get medication via prescription
Lead Interaction Designer
Lead UX Researcher
Product Owner
Business Analyst
User Researchers x2
3 months
In detail
In the U.K there are various ways for NHS patients to obtain, use and manage their medication. The journey involves many actors and systems that complicates what should be a straightforward process. Patients talk of stress and confusion. For the NHS, this means a lot of uncollected medication that costs money which could be spent elsewhere on improving the health service.
At the kick off meeting the team was given the following problem statement:
How might we
Empower patients to have increased choice and flexibility over how they obtain and manage their medication, using digital solutions to support a paperless NHS.
Before any work had begun, the team felt that this problem statement was far too broad to successfully run a discovery within time period. The original problem statement wanted to explore how people obtain, manage and use their medication - the complete medication journey. We felt that each part of this journey could be separated into individual discoveries, such was its breadth.
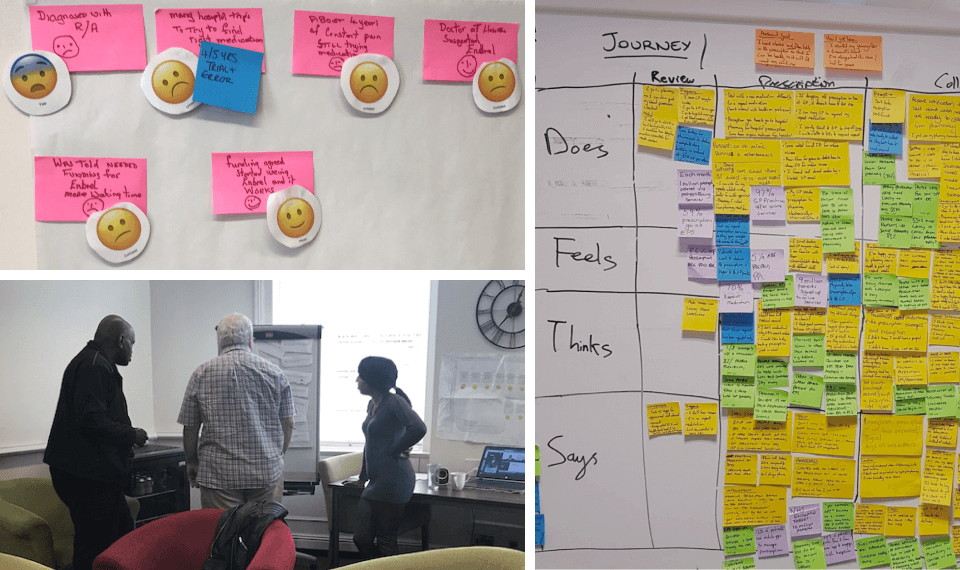
In order to prove that the problem was too large, I led a team consisting of a product manager, BA and researcher in conducting 4 participatory workshops, with 22 participants, throughout the country in 10 days. We wanted to learn about patient’s prescription journeys. Participants talked through and mapped out their complete medication journey, whilst at the same time highlighting things that worked and the issues they faced.
I had already sold the team on using the Jobs-To-Be-Done (JTBD) framework, so I tailored our line of questions to drill down into the context, situations, motivations of the patients throughout their journeys.
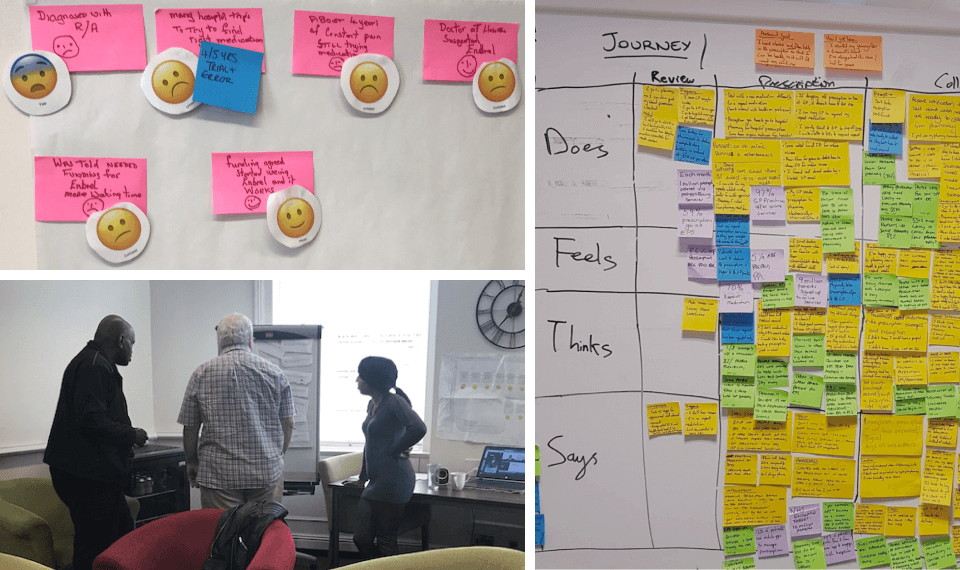
During analysis and synthesis of our findings, we mapped the patient journey with the four elements of an empathy map to help us see the complete end-to-end picture and where the main pain-points or area of focus were. Most of the insights that were uncovered were focused on the process of patients obtaining their medication.
Insights
With most of the pain points that we discovered being around how patients obtained their medication, we had validated our assumptions that this discovery needed to focus on one specific problem. The research helped us revise the problem statement to:
How might we
Make medication more convenient to obtain for patients with repeat prescriptions.
I organised regular show and tells with the wider directorate to present our findings, storyboards and experience maps (to bring to life the problems that patients faced) and introduce the revised problem statement.

I enjoy looking at different ways of working. It allows for continuous personal development and to experiment with new ideas. I recommended to the team that we adopt a slightly different approach and introduced JTBD. We used this framework during our research to help us uncover the jobs that patients wanted to do with regards to their prescription journey.
Example job to be done
When I am about to collect my medication from a nearby dispenser, I want to see which dispensers have my medication in stock, so I can be confident I'll only have to go to one dispenser to collect my medication.
It was a fun exercise and one which myself and team learnt a great deal about. It was quite a task though. Highlighted by the 88 jobs we discovered, which we eventually narrowed down to a still exceptionally large number of 64. We did however prioritise these into the top 10 to focus our ideas around, with a card sort and patient interviews.
My colleague, Luke Johnson, wrote a great piece on our experience with JTDB.
With the prioritised list of jobs in hand, I facilitated a co-creation workshop with stakeholders. We presented our findings to date and used design thinking workshop methods, based around the patients jobs, to create many ideas. We converged on one or two ideas which we wanted to build concepts around.
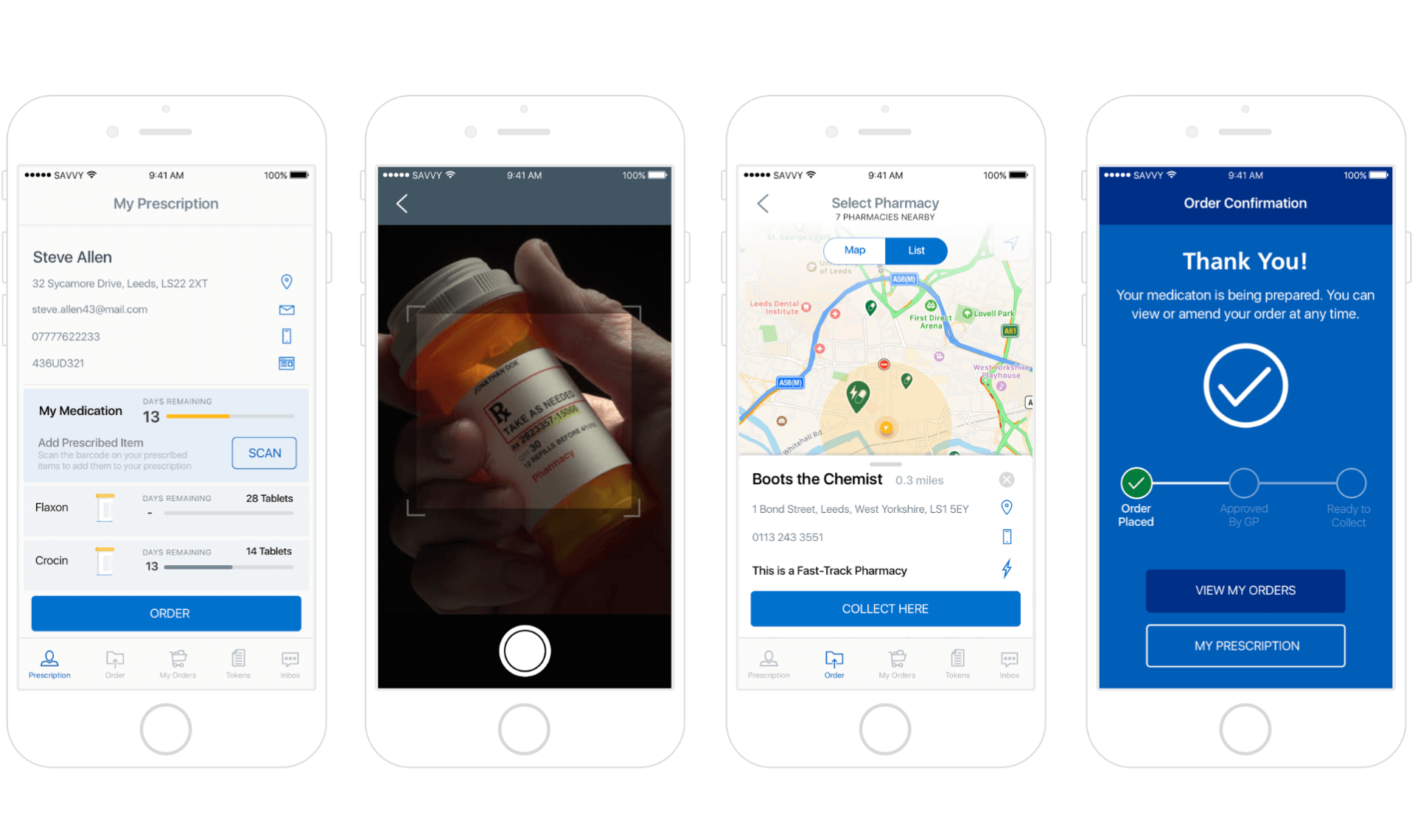
The concept was centred around an app that would let patients order their repeat medication. It gave them complete control and flexibility in terms of ordering, collection method and location.
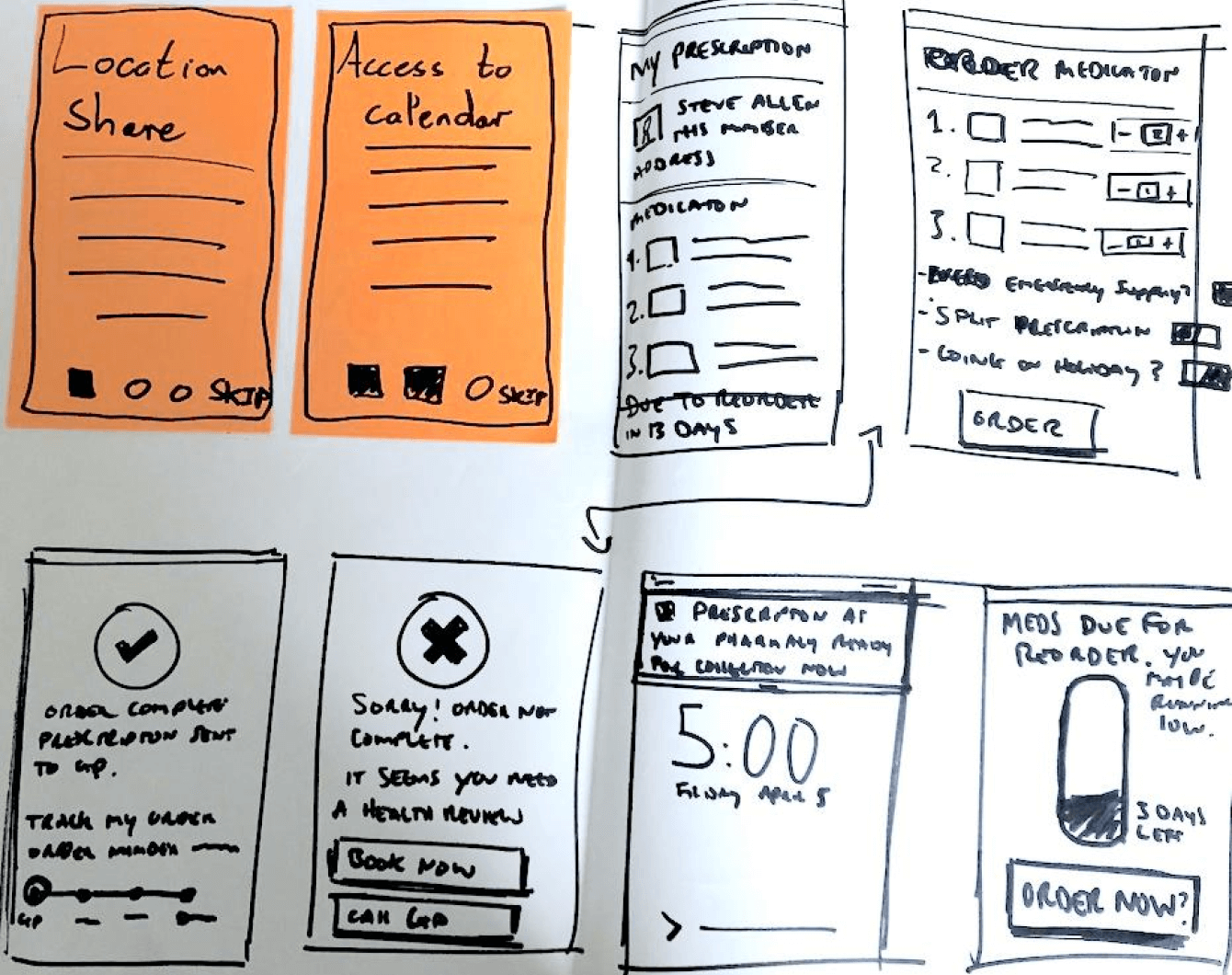
We sketched out a possible UI and then I mocked up a simple wireframe. All of our ideas, though based on solid insight (and patient jobs), had some form of assumption attached to them. In order to mitigate risk we identified the riskiest assumptions and tested them first in lo-fidelity. I felt that this was a good balance between making it feel like an app yet it took only a day to create and was easily updatable based on the feedback we would recieve.
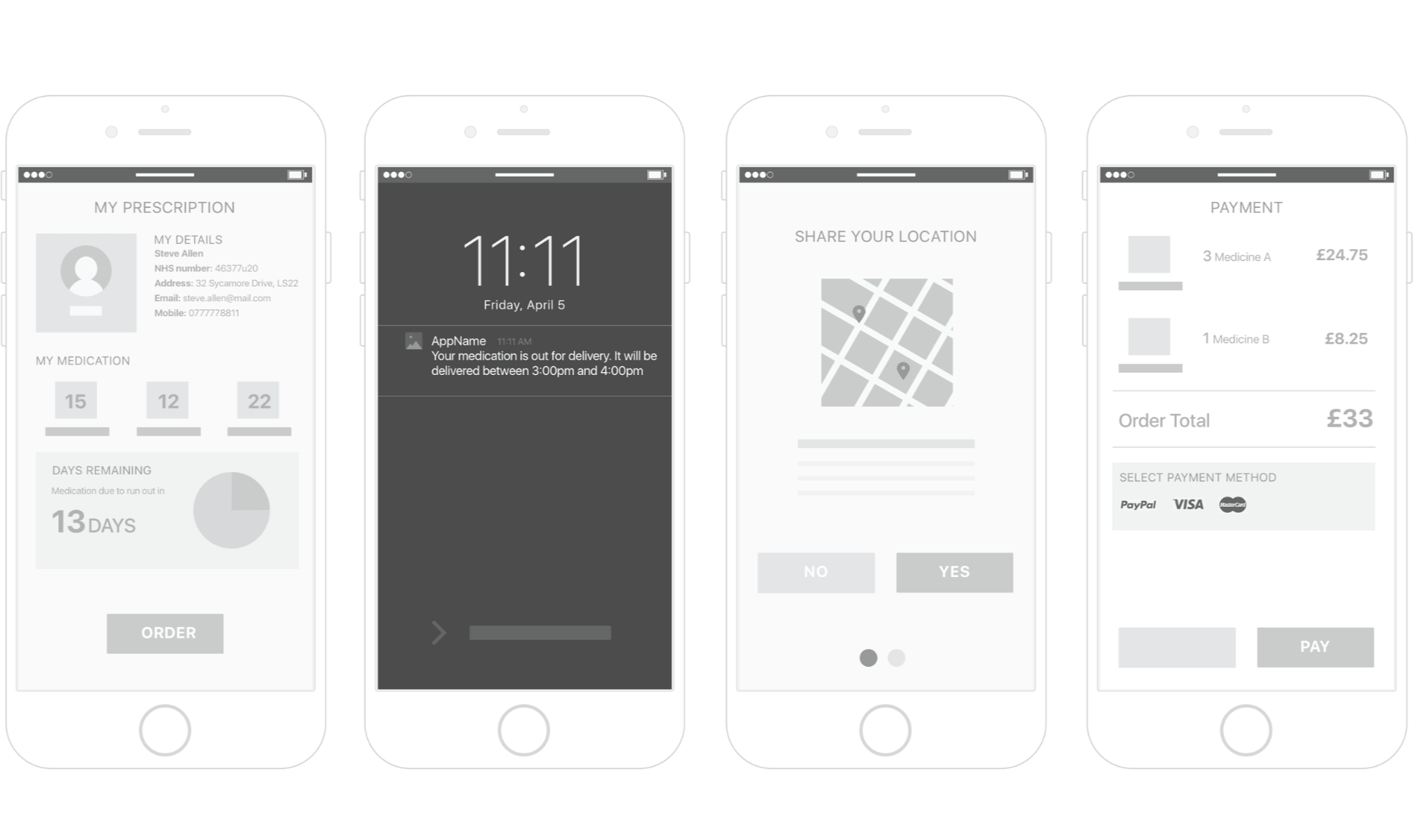
I created a clickable, linear prototype using InVision (and then for subsequent iterations Marvel). I put this on a device then myself and colleagues conducted concept testing with 10 participants (various demographics). We visited people at their homes, in pharmacies and GP waiting rooms. We felt the contextual nature would allow us to gain insight not only around their reception to the concept, but to understand how they go about getting their medication currently and how this may change in future with the proposed concept.
Insights
Whilst the initial concept had been well received with people asking when this would launch, I knew that it was only a small number of patients and we had many more assumptions to test out and iterate the concept based on the insights we had dsicovered.
Additionally, I noted that whilst some participants understood it was a mobile app concept, there were many people, even those considered tech savvy, that weren’t resonating with the idea. I decided that we need to up the fidelity. I built out more of the UI and pieced it together to create an interactive prototype.
We spent the next couple of weeks iterating and testing out assumptions until we reached a point where we were confident of the concept that we had.
This is great. It means I don't have to wait around in a chemist. It looks so easy to order my prescription and I can pick and choose when and where to get them. When did you say this will come out?
The discovery was coming to a close and it felt like we had found a nice conclusion to share everything we had discovered. If such a service existed, then users felt it would serve their needs (jobs), make the repeat prescription journey much easier and more convenient.
By thoroughly researching the problem space, we made an early call to focus only on one aspect of the patient medication journey. This allowed us to successfully deliver a discovery that enabled the directorate to showcase how they might launch a service which would benefit patients.
This was never about us delivering a final product or service. It was about enabling other internal teams and third party suppliers to access our research to help them shape their own solutions.
We shared this project with the team responsible for the NHS App who have since implemented a version of this into the live service, albeit minus some features. We presented at the Pharmacy show 2017, which triggered a great response from the audience and third parties. Off the back of this we were invited to present to the teams at Well Pharmacy and Co-op Pharmacy. This open sharing of work meant they could use our findings and ideas to help them make their own service experience better.
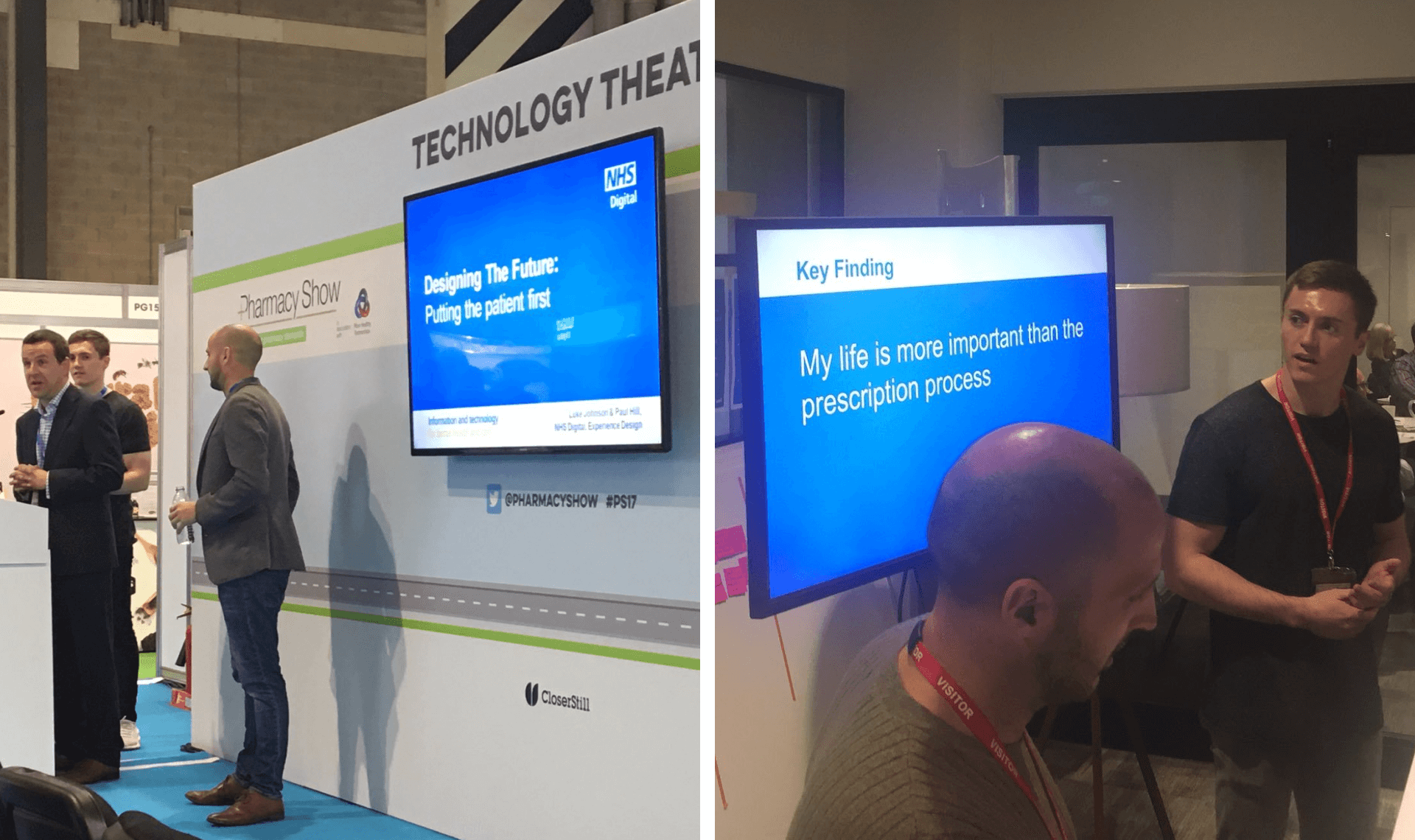
Looking forward to hearing from the 'best double act in NHS Digital' #ps17 @NHSDigital
Nodding along to @NHSDigital talk here @well_digital.